Traumatic Brain Injury
Traumatic brain injury is a direct (impact to the head) or indirect (shaking as in whiplash or “shaken baby”) mechanical injury to the brain that results in tearing, stretching, or shearing of tissue, secondary inflammation, and neurological dysfunction. Current estimates are 4.8 million cases yearly in the United States, 75% of which are mild TBI (concussion). Over 50,000 people die in the U.S. every year from severe TBI.
What are the effects?
Traumatic brain injury is characterized by altered consciousness or loss of consciousness with varying severities of injury (mild, moderate, or severe) that are proportional to the force of injury and cause anywhere from temporary neurologic dysfunction to death. Up to 55% of all mild TBI patients develop the persistent post-concussion syndrome characterized by cognitive symptoms, headache, irritability, sleep disruption, fatigue, dizziness, depression, anxiety, apathy, and change in personality.
Benefits from HBOT
HBOT is the only therapy that directly treats the underlying disease processes of TBI (decreased oxygen, decreased blood flow, swelling of the brain, constriction of blood vessels, acidosis, anaerobic metabolism). HBOT has been shown in multiple studies to have the greatest reduction in mortality of any therapy. One to three sessions of HBOT in the acute period can decrease the mortality by 50-60% (see Rockswold review below). There is very little published experience of HBOT in mild TBI, but in Dr. Harch’s career he has treated many patients within the first week after concussion/mild TBI. With just a few treatments at our clinic, most patients experience near complete or complete relief of symptoms. For patients with the persistent post-concussion syndrome, HBOT is the most effective therapy known. Dr. Harch has shown that HBOT is effective in relieving symptoms in both civilian and military blast-injured patients, and that HBOT causes a reduction in suicidal ideation in veterans.
Case Study
See Curt Allen’s story here.
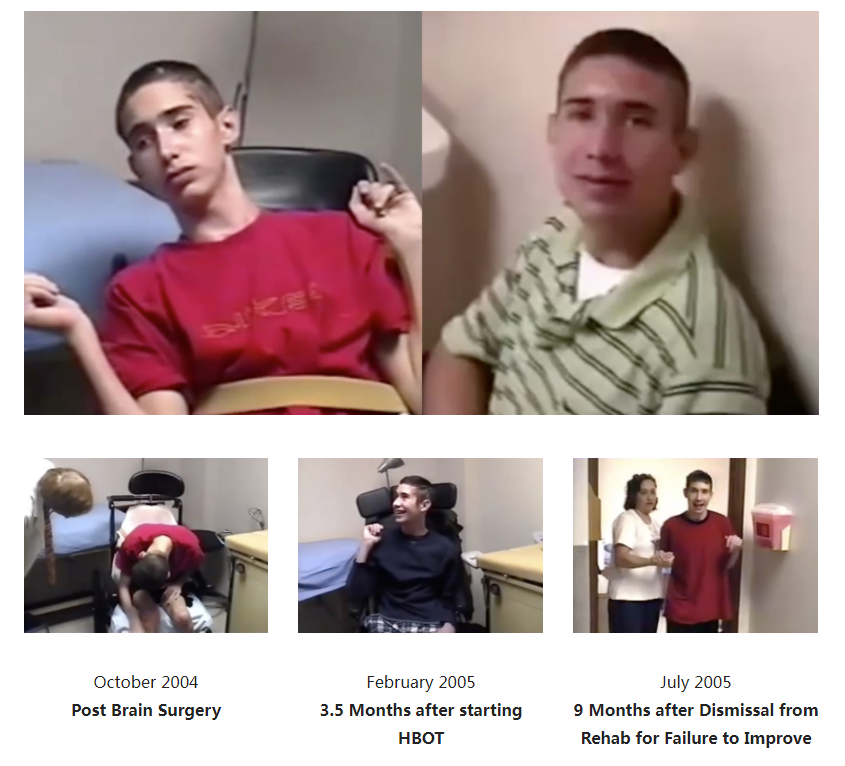
Geoffrey was a 19 year old young man who was involved in a severe motor vehicle accident on an icy winter night in 1989. He was comatose at the scene, spent weeks in the ICU on a ventilator, and then months in a rehabilitation hospital. He was discharged to home and the care of his mother with inappropriate social behavior, cognitive deficits, and repeating sentences in conversation, and he required round-the-clock supervision. His repetitiveness was a particular stressor for his parents, and they were seeking institutional placement for Geoffrey. He was referred for evaluation for HBOT nearly 3 years after his accident.
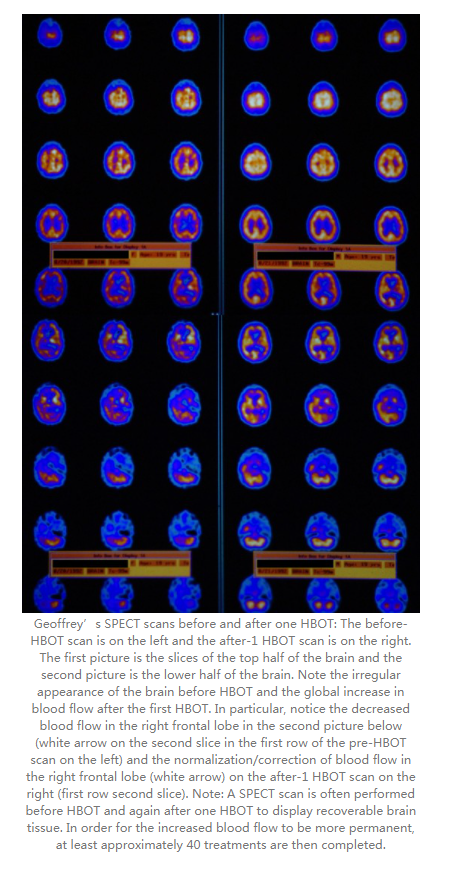
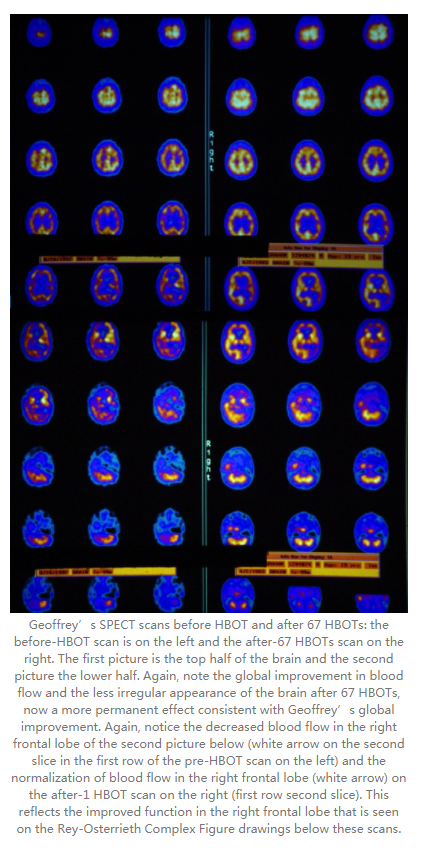
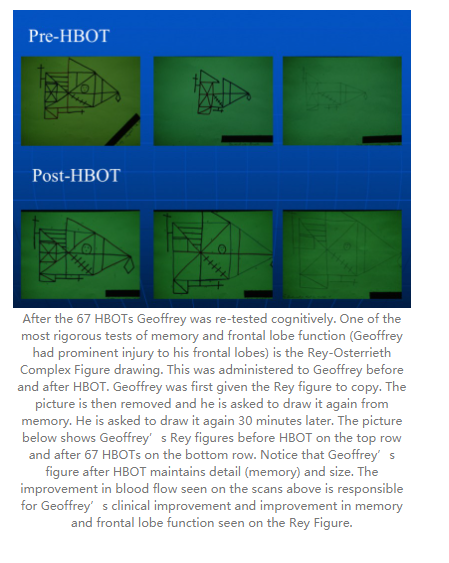
Geoffrey had a SPECT scan, a single HBOT, and a repeat SPECT (see below) which showed a dramatic improvement in brain blood flow. This evaluation was followed by 67 HBOT treatments over the course of the next 8 months, which were delivered in multiple blocks. At the end of treatment, the patient had marked improvement in his behavior, perseveration (repetitive speech), cognitive deficits, and no longer required round-the-clock supervision. Repeat cognitive testing showed improvements in memory and other functions. He was advanced to assisted living and part-time employment. Periodically, Geoffrey returned for additional short courses of HBOT. When asked why he continued to come to New Orleans for HBOT, Geoffrey responded, “I feel so much better in my head and can do new things when I have HBOT.”
Supportive Research and Information
https://www-ncbi-nlm-nih-gov.ezproxy.lsuhsc.edu/pubmed/29132229 (Rockswold review).
https://www-ncbi-nlm-nih-gov.ezproxy.lsuhsc.edu/pubmed/29152209 (Dr. Harch’s study in veterans with blast TBI and PTSD. The discussion section includes a review of all of the HBOT studies in mild TBI persistent post-concussion syndrome).


 +86 13621894001
+86 13621894001
 rank@macy-pan.com
rank@macy-pan.com
 +86-+8613621894001
+86-+8613621894001


 Tel:
Tel: Mob:
Mob: WhatsApp:
WhatsApp: Email:
Email: Add:Bldg 15, No.889 Guinan Road, Songjiang District, Shanghai, China
Add:Bldg 15, No.889 Guinan Road, Songjiang District, Shanghai, China